Editorial Disclaimer
The views expressed in articles published on FIRES do not necessarily reflect those of IES or represent endorsement by the IES.
By Douglas Steel, Ph.D., NeuroSense
The purpose of this article is to evaluate from a biological standpoint the rationale for the establishment of a Circadian Lighting standard put forward by UL under the direction of Dr. Mark Rea of the Lighting Research Center at Rensselaer Polytechnic Institute. This critique is limited in scope but also applies to utilization of the Circadian Stimulus (CS) calculator also developed by the LRC.
A fundamental concern is that the proposed UL guideline and associated utilization of the CS and WELL calculations are misrepresenting a scientific “Model” as a theory or tool that can be practically applied in the field.
In the process of scientific discovery, it is understood that not all of the knowledge about a particular phenomenon will be available at the outset. It takes a process of conducting numerous experiments of trial and error and repetitive iteration for scientists to develop hypotheses that account for all observed outcomes. It is through the creation of a model that the scientific community collects data, make predictions and assumptions, and tests that model against actual observations.1 Over time, the sophistication of models improves, and some continue to hold up to challenges from new data, while others fail and require modification or rejection. We are all familiar with the process of model testing, as both climate change theory and evolutionary theory have been proposed and tested. The controversy arises when one asks the question “at what point do we know enough to declare that a model is representative of fact?”
Turning to the issue of the proposed UL Circadian guidelines, what is being proposed is really just a model that has been constructed in an attempt to consider some (but not all) of the factors that can collectively account for the human body’s response to light exposure with respect to Circadian factors. In this case, data from different sources have been combined to form hypotheses, which it is hoped will continue to be refined in order to increase our understanding of biological responses. This will then inform the design and execution of new experiments, the results of which continue to refine the model until we have a predictive working model of how a physiological process responds to inputs, with defined outputs. At that point, with consensus reached in the scientific community, the model could then be considered a theory or tool, in that it could be used predictively to achieve a specific outcome.2
I would argue that the UL and referenced CS “tools” are in fact still an unvalidated or improperly validated model in that it has not gone through a process of rigorous testing. In addition, a number of essential factors that contribute to circadian patterning have (as acknowledged by the LRC) not been included in the model (e.g., light exposure history and duration patterns). Thus, the model is known to be incomplete and unvalidated. Yet, for some reason it has been released to the lighting community by the LRC as a tool ready for use in the field. I believe it is the responsibility of UL and the LRC to issue a public statement regarding the CS “tool,” clarifying that it is at this stage of development a rudimentary model along with specific appropriate bounds for intended use—as a model by the lighting research community.
In what ways do the UL Guideline and CS calculator fail as tools?
- The proposed model calls for a recommended light exposure of 254 lux of vertical illumination for 2 hours in the morning upon the surface of the eye. The specification of an arbitrarily precise number such as 254 lux is invalid and misleading because it does not specify the spectral power distribution of the light to be used for exposure, and it does not account for numerous physiological factors. The actual functional consequences of light exposure upon circadian phenomena occur inside the eye, beginning with exposure of rods and cones in the retina, and intrinsically photosensitive retinal ganglion cells (ipRGCs) in the ganglion cell layer. It is well established that the lens of the eye turns increasingly yellow with age3 (see Figure 1). Thus, less light (particularly at the blue end of the spectrum) reaches the retina. A value of 254 lux has little functional relevance to the elderly.
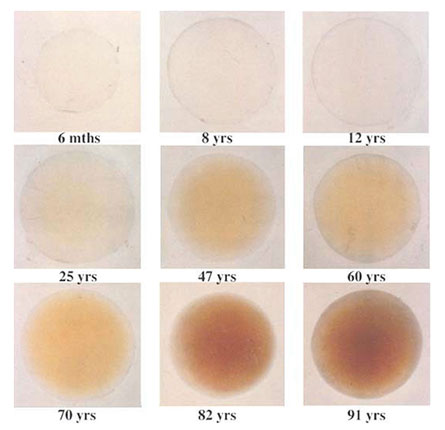
Figure 1. Yellowing of the human lens of the eye with age.3 Thus, any recommended exposure guidelines must reflect and compensate for differing degrees of yellowing of the lens of the eye with the age of the occupant, or the effects of individual differences that will affect the functional response. Otherwise, the desired responses may be erroneous. In addition, the model does not provide guidelines for use in environments where multiple occupants are of widely differing ages.
- The premise of the proposed UL standard is based upon a set of “circadian-effective lighting design criteria” (lines 119 – 126 in the proposed standard). This tool is the work product of the LRC, and is known as the Circadian Stimulus Calculator. It has not been critically and independently reviewed by independent researchers in the scientific community, and certain specific assumptions made by this “tool” are outside the bounds of testability. In order to be elevated to a working standard, a consensus of the relevant scientific community must test and determine whether the outcomes predicted by the models are accurate, precise, reliable, and valid.
- The proposed UL standard and CS Calculator do not take into account any light exposure (i.e., photic history) occurring in the home or other settings after daylight hours. It is well established that excessive blue light exposure in the evening has a deleterious effect on sleep onset, sleep quality, circadian entrainment, and alertness and arousal throughout the daily schedule. In what way can a proposed exposure of 254 lux in the morning compensate or account for light exposure patterning in the evening? In addition, this model does not (and cannot) account for supplemental exposure to blue-enriched light emanating from cell phone, tablets, computers, and TVs in daytime and nighttime settings. While any metric would be challenged to provide such an accounting of individualized light exposure, no recommended guideline or formula for calculating circadian exposure can claim to be valid without these measurements.
- The proposed UL standard and CS Calculator rely on predicted melatonin suppression at night, and assume that it is a valid marker for estimating circadian effects of light exposure. Under this model, melatonin is acting as a proxy biomarker for melanopsin responses in the eye in mediating suprachiasmatic nucleus (SCN) responses. Neither melanopsin nor melatonin is actually measured as part of conforming to this standard. Further, the estimated degree of melatonin suppression is being inferred from one or two datasets generated over 15 years ago.4, 5 It is dangerous to deduce the present-day health status of human beings based on estimated melatonin suppression inferred from old datasets, dating from a time before LED lighting was in commercial use. It is not yet known whether different spectral power distributions (SPD) of different light sources having the same correlated color temperatures (CCT) would cause different responses in the patterning of melatonin suppression. Thus, this could potentially yield erroneous results from the CS Calculator.
- It has not been clearly established that melatonin is even a valid biomarker for melanopsin actions. In order to make that inference, one would have to establish that melatonin is accurate, precise, reliable, and valid as a biomarker, according to the standards of Clinical Chemistry and Chemical Pathology as regulated by the FDA in the Medical Science Community.6 The pathway by which light exposure results in melatonin responses is a long and circuitous one (see Figure 2), involving multiple brain regions and many steps of modulation by other chemicals and brain functions. The proposed UL Guidelines and CS Calculator do not account for the functional consequences of modulation of this pathway. Thus, certain patient populations on particular prescription medications that modulate neurotransmitters—including norepinephrine, serotonin, and gamma-aminobutyric acid (GABA)—might be expected to display different responses to light exposure. Architects, designers, and anyone else who uses these models as tools may be unwittingly engaging in modulation of human biological processes using an unvalidated and highly inaccurate model. This could result in harm to individuals predisposed to conditions such as migraine, epilepsy, photophobia, photosensitivity, or pathologies involving sensory processing disorders.
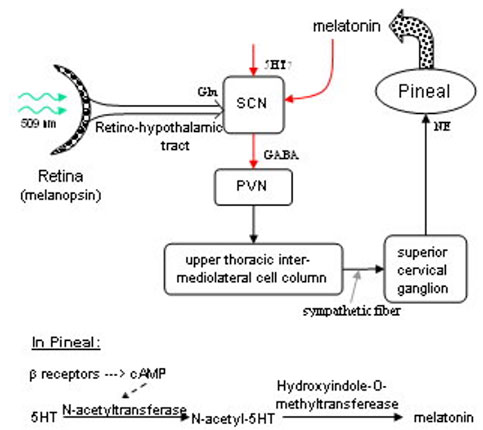
Figure 2. Neuroanatomy and neurochemistry of the pathway connecting ipGRCs to melatonin release.7 - Even if melatonin is justifiably used as a proxy for melanopic response, to infer that this can account for circadian entrainment processes is incorrect. While the SCN receives inputs from the eyes via the ipRGC-mediated pathways, other neural pathways that have nothing to do with light exposure also modulate SCN function. A recent review cites a number of distinct input pathways to the SCN (see Figure 3).8 These include the medial and dorsal parts of the raphe-dorsal hypothalamic pathway mediating arousal, social cues, and feeding information, and a mixed-photoreceptor responsive pathway projecting from the intergeniculate leaflet to the SCN.9
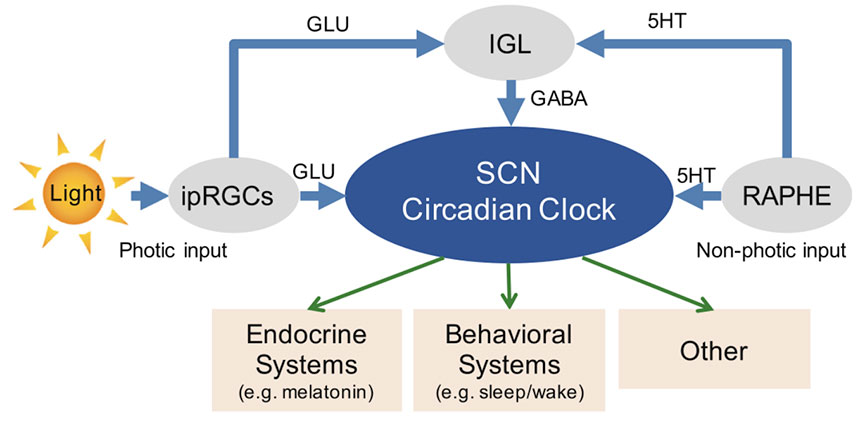
Figure 3. Multiple pathways in addition to ipRGCs modulate SCN circadian functions.9 - It is not appropriate to use correlated color temperature as an approximation of the spectral power distribution of a luminaire since it does not provide any information as to the fractional contribution of any specific part of the spectrum (particularly blue light). Without making an estimation of the extent of relative ipRGC stimulation, there is no way that a circadian effect can be predicted.
- The idea that there can be a “specific recipe” for human-centric lighting that can be universally applied to all persons is unrealistic because of the tremendous variability between individuals based on age, setting, genetics, environmental factors, individual physiology, and personal behaviors such as coffee or alcohol consumption, ambient lighting preferences, and undesired exposure from other ambient light sources. While many of these factors could potentially be accounted for as models such as these become increasingly sophisticated, no effort has been made to do so. It is easy to envision the specification of a “general performance envelope” of factors that would apply to a majority of persons in any given environment, but such an envelope has been neither defined nor proposed.
- Any “theory,” “tool” or “metric” that emerges from the development of a model must be predictive, verifiable, and, from a practical standpoint, measurable using instruments or based upon provided mathematical values. As it stands, the UL Guideline and the CS Calculator are neither predictive nor verifiable because it they are not based on the direct measurement of any parameter, dependent measure, or independent measure. Predictiveness is a measure of compliance to an expected outcome, yet no statement of a means of assessing an outcome (or the bounds of such) is provided. The declaration that the metric is measurable using standard equipment is also flawed; while one can measure the exposure metric under controlled conditions, it is much more challenging to measure it in real-world settings where the contribution of multiple light sources must be considered. Further, as previously stated, no outcome metric or measured value is recommended or provided.
Those of us involved in the study of lighting effects on living organisms, and in translating those discoveries into practical applications and creating delivery devices encourage and welcome the development of guidelines that define exposure conditions to achieve specific biological outcomes. However, this cannot be achieved by ignoring significant parts of the biological mechanism, or by stating an arbitrary value without providing means of measuring and validating outcomes. There is no value to the lighting industry in taking shortcuts and utilizing overly simplistic and naïve models to pretend that we have a degree of knowledge that is currently lacking. We are certainly capable of modulating human responses to light exposure, but we must hold ourselves to a higher standard of knowledge and expertise.
In conclusion, the proposed UL criteria for circadian entrainment are inadequate, inaccurate, misguided, based on a lack of understanding of fundamental neuroscience, and utilize an untested and questionable “CS Calculator” (see companion article by Ian Ashdown). While it is worthwhile to establish standards in a given field, the time has to be right based upon our necessary understanding of the mechanism’s underlying phenomena. The proposed standard and methods of calculation do not follow accepted standard methods of scientific investigation and documentation of physiological phenomena.
References
1 https://en.wikipedia.org/wiki/Scientific_modelling
2 https://bscdesigner.com/all-about-the-scientific-method.htm
3 Lerman S. Radiant Energy and the Eye. London: Macmillan; 1980.
4 Thapan K, Arendt J, Skene DJ. An action spectrum for melatonin suppression: Evidence for a novel, non-rod, non-cone photoreceptor system in humans. J Physiol. 2001;535(Pt 1):261-7.
5 Brainard GC, Hanifin JP, Greeson JM, Byrne B, Glickman G, Gerner E, Rollag MD. Action spectrum for melatonin regulation in humans: Evidence for a novel circadian photoreceptor. J Neurosci. 2001;21(16):6405-12.
6 https://www.fda.gov/medical-devices/products-and-medical-procedures/vitro-diagnostics
7 http://flipper.diff.org/app/items/info/2474
8 Silver R, Rainbow M. (2015) The suprachiasmatic nucleus and the circadian timekeeping system of the body. In: Pfaff DW (ed.), Neuroscience in the 21st Century. New York: Springer; 2015:1-49.
9 Cao D, Barrionuevo PA. J Solid State Lighting. 2015;2:10.

