This page provides you with a simplified way to quickly see the FAQs contained in the IES Photobiology Committee’s Committee Report CR-2-20-V1. The full Report contains supporting information on this topic as well as an introductory video. These FAQs have been vetted through our ANSI-approved standards development process through a consensus of volunteers representing varied viewpoints and interests. The IES makes no guaranty or warranty as to the accuracy or completeness of information contained in these FAQs, and disclaims liability for any injury to persons or property or other damages of any nature whatsoever resulting from the use of or reliance upon this information. The reader is directed to the full Report for more background, references and summary information on this topic.
Download Committee Report CR-2-20-V1 [PDF 1.3MB]
For questions on IES Committee Report CR-2-20 FAQs, email uvgi@ies.org.
1.0 Basic Questions
1.1 What is germicidal UV, and what is UVGI?
Germicidal UV (GUV) refers to using ultraviolet radiant energy to inactivate bacteria, mold spores, fungi or viruses. When the process is applied in a given location, it has generally been referred to as ultraviolet germicidal irradiation (UVGI). Because of the public’s concern about ionizing radiation (e.g., X-rays and gamma rays), the term GUV avoids needless concerns about a link with that type of radiation. Another non-technical term is germicidal light, although “light” is technically only visible radiation.
1.2 Is all ultraviolet considered germicidal ultraviolet (GUV)?
No. Germicidal ultraviolet (GUV) – refers to short-wavelength ultraviolet “light” (radiant energy) that has been shown to kill bacteria and spores and to inactivate viruses. Wavelengths in the photobiological ultraviolet spectral band known as the “UV-C,” from 200 to 280 nanometers (nm), have been shown to be the most effective for disinfection, although longer, less energetic UV can also disinfect if applied in much greater doses. UV-C wavelengths comprise photons (particles of light) that are the most energetic in the optical spectrum (comprising UV, visible, and infrared) and therefore are the most photochemically active. (See Figure 1.)
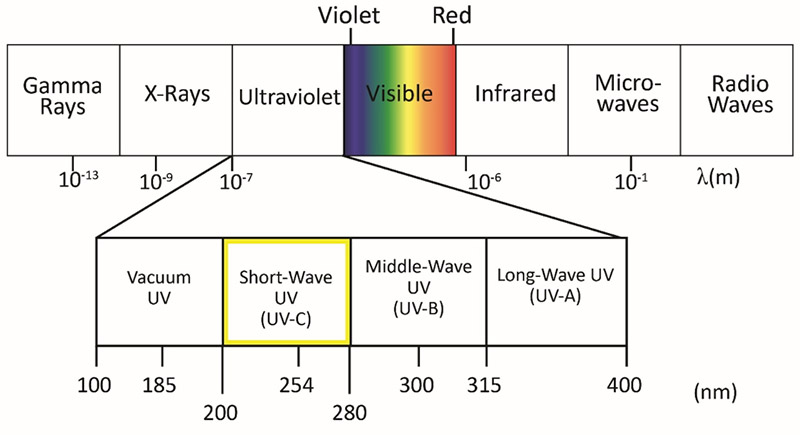
Figure 1-1. The ultraviolet portion of the electromagnetic spectrum 1.3 Can UV-C kill viruses as well as bacteria?
Yes, UV-C kills living bacteria, but viruses are technically not living organisms; thus, we should correctly say “inactivate viruses.” Individual, energetic UV-C photons photochemically interact with the RNA and DNA molecules in a virus or bacterium to render these microbes non-infectious. This all happens on the microscopic level. Viruses are less than one micrometer (µm, one-millionth of a meter) in size, and bacteria are typically 0.5 to 5 µm.
1.4 Can UV-C effectively inactivate the SARS-CoV-2 virus, responsible for COVID-19?
Yes, if the virus is directly illuminated by UV-C at the effective dose level. UV-C can play an effective role with other methods of disinfection, but it is essential that individuals be protected to prevent UV hazards to the eyes and skin as elaborated in Section 4. UV-C should not be used to disinfect the hands!
1.5 Can near-ultraviolet (UV-A) lamps, such as UV insect traps, be used for GUV?
No. UV-A and longer (visible) wavelengths do not have germicidally effective emission wavelengths to inactivate viruses. Their relative disinfection capability is very minimal on the order of 1,000 times less effective in terms of fluence rate than the low-pressure mercury germicidal lamp. There have been only very special applications of wavelengths in the UV-A and violet (e.g., 405 nm), which require very high doses not practical in an occupied environment and were not recommended for viral sterilization. The trace amount of UV-B that is emitted from some white-light fluorescent lamps probably has similar efficacy.
Light-emitting diodes (LEDs) have been available for some time in the UV-A region. The advantage of UV-A or visible-light LEDs would be that they can easily be incorporated into LED-based luminaires, and there might be no need for protective gear. However, the efficacy of violet or UV-A energy that is not harmful to the skin or eyes is minimal.
1.6 What about UV-B lamps for GUV?
UV-B (280 to 315 nm), particularly the shorter wavelengths near 300 nm and below, can be relatively effective as a germicidal source, but in accidental exposures there is a significantly higher risk for severe sunburn and even delayed effects for both skin and eyes, because UV-B penetrates the skin more deeply.
1.7 Does the ultraviolet in sunlight have a GUV effect?
Yes, particularly in the late spring and early summer when the sun is high in the sky and the UV index is high. At a UV Index of 10, the duration to achieve at least a three-log kill of bacteria (99.9% killed) is estimated as less than one hour.[5]
[5] Lytle CD, Sagripanti J-L. Predicted inactivation of viruses of relevance to biodefense by solar radiation. J Virol. 2005;79(22):14244-52.
2.0 Medical and Healthcare Questions
2.1 How is the COVID-19 virus spread?
The official position of the World Health Organization (WHO) is that this virus is spread by contact with large respiratory droplets, directly or indirectly by touching contaminated surfaces and then touching the eyes, nose, or mouth. However, research is underway to determine the degree of airborne spread—meaning virus in particles so small that they remain suspended in air. Such aerosol results from the evaporation of larger respiratory particles generated by coughs, sneezes, ordinary speech, singing, and possibly by faulty plumbing systems, as occurred with the severe acute respiratory syndrome (SARS) virus. How much of the virus responsible for COVID-19 is spread by the airborne route is not clear, but recommendations for healthcare workers to use fitted respirators, not surgical masks, reveal official concern for airborne transmission. The possibility that inhaled virus may result in more-severe lung damage than acquisition by other routes—for example, via the mouth, nose, or eye—is currently being investigated.
2.2 How long do virus particles and bacteria remain airborne?
This is important, but difficult to answer in a simple fashion and it depends on how the microbes were made airborne, e.g., from a sneeze or cough, or by being blown up from surfaces or dusted off clothes. The smallest particles (1- to 5-µm droplet nuclei) can remain airborne much longer than cough droplets—for many minutes or even hours.
2.3 How can airborne spread viruses be reduced?
Diagnosis of infectious cases and their isolation is a critical intervention, but transmission from asymptomatic persons is believed to play an important role in community transmission. In the U.S., the Centers for Disease Control and Prevention (CDC) has recommended that everyone wear non-medical face covers to reduce spread by respiratory droplets, both large and small. Heathcare workers should wear well fitted respirators designed to exclude airborne particles, in addition to following all contact precautions. For the airborne component, ventilation, social distancing, and other means of air disinfection are expected to have a role. Natural ventilation outdoors and in homes can be highly effective where conditions are optimal in terms of airflow and temperature. Mechanical ventilation can be effective, but 6 to 12 air changes per hour (ACH) are recommended in general for air disinfection or dilution.
Upper-room GUV air disinfection is a primary means of safe and highly effective air disinfection, provided it is planned, installed, commissioned, and maintained according to current international standards. A knowledgeable consultant is recommended. Room air cleaners, disinfecting air through HEPA filters, in-duct UV lamps, or other methods seem attractive, but their clean-air delivery rate when converted to room ACH is often trivial—no more than 1 or 2 added ACH. GUV in-duct air disinfection is a secondary approach to treating any recirculated air.
2.4 How does GUV work to disinfect air?
Commonly used GUV lamps generate predominantly 254-nm UV radiant energy, which is close to the peak germicidal wavelengths of 265 to 270 nm – both in the UV-C range, compared to the longer-wavelength ultraviolet (UV-A and UV-B) in sunlight. GUV radiant energy damages nucleic acids (DNA and RNA), thus preventing replication and leading to the death of virtually all bacteria and inactivation of all viruses—both DNA and RNA types. Bacteria and viruses vary somewhat in UV susceptibility, with environmental organisms, fungal spores, and mycobacteria being relatively harder to kill than more rapidly replicating and non-environmental microbes and most bacteria. But even fungi are effectively killed with high-dose UV, which is used, for example, to treat fungal contamination of air conditioning systems. GUV can be most effectively used to disinfect air in the upper room where ceiling height permits, but can also be used in ventilation ducts and room air cleaners, as noted. As explained below, upper-room GUV is considered the most effective application for room air disinfection, where feasible.
2.5 Has GUV been useful in medical treatment facilities?
Yes. Some hospitals have used portable GUV fixtures to disinfect air and surfaces in unoccupied, locked rooms as a supplemental control measure to reduce the spread of healthcare associated infections.[6] However, well controlled studies of efficacy are very difficult to conduct and therefore lacking. Medical treatment facilities are using GUV in three primary ways: 1) upper-room GUV fixtures with air mixing, for controlling airborne pathogens in an occupied space; 2) mobile GUV units, to disinfect high-touch surfaces; and 3) GUV in HVAC air handling units, to treat recirculated air and to reduce mold growth on cooling coils. Autonomous (“robot”) systems have been used in some U.S. hospitals and were used in the People’s Republic of China in response to COVID-19.[7] In fighting a war, which this is seen to be, a single weapon is never used; rather, multiple weapons in the armamentarium are exploited.[8] There is no reason not to make full use of GUV with appropriate precautions in this “war” against COVID-19.
[6] Wight W. Germ-killing robots fight drug-resistant pathogens at Army hospitals. 65th Medical Brigade Public Affairs Office. 24 Jul 2017. Online: https://www.army.mil/article/191241/germ_killing_robots_fight_drug_resistant_pathogens_at_army_hospitals. (Accessed 2020 Feb 28).
[7] Ackerman, E. Autonomous robots are helping kill coronavirus in hospital. IEEE Spectrum. 11 Mar 2020. Online: https://spectrum.ieee.org/automaton/robotics/medical-robots/autonomous-robots-are-helping-kill-coronavirus-in-hospitals. (Accessed 2020 Mar 16).
[8] Lee T, Jordan NN, Sanchez JL, Gaydos JC. Selected nonvaccine interventions to prevent infectious acute respiratory disease. Am J Prev Med. 2005;28(3):305-16.
2.6 Can whole-room UV-C effectively inactivate the SARS-CoV-2 virus responsible for COVID-19?
While UV-C could be a secondary infection control measure for disinfecting potential germ-carrying deposits on accessible (not-shadowed) surfaces, its great value would be in disinfecting air in areas where this may be a concern (e.g., intensive care wards, hospital intake facilities [or tents]). Upper-air GUV is the safest, most effective application of UV-C. In special locations, where viral transmission is highly likely, whole-room UVGI (from suspended fixtures directing UV-C downward) could be applied, provided strict precautions can be followed. It is critical that any persons remaining in the space being disinfected from overhead and side UV-C lamps wear protective clothing and eye protection, or exposure to harmful UV will occur. Whole-room GUV has been safely applied in unoccupied rooms where entry is forbidden during the UVGI.
2.7 Does the CDC recommend GUV in healthcare facilities?
In the U.S., the Centers for Disease Control and Prevention (CDC) has provided guidelines for the use of UVGI lamps in upper rooms and air handling units (AHUs) as a supplemental control measure for air disinfection.[9, 10, 11]
[9] Sehulster L, Chinn RYW. Guidelines for environmental infection control in healthcare facilities – Recommendations of the Centers for Disease Control and the Healthcare Infection Control Practices Advisory Committee (HICPAC). 2003;52(RR10):1-42.
[10] Jensen PA, Lambert LA, Lademarco MF, Ridzon R. 2005. Guidelines for preventing the transmission of Mycobacterium tuberculosis in health-care settings, 2005. Morbid Mortal Weekly Rep. 2005;54(RR17):1-141.
[11] Centers for Disease Control and Prevention; and National Institute for Occupational Safety and Health. Environmental Control for Tuberculosis: Basic Upper-Room Ultraviolet Germicidal Irradiation Guidelines for Healthcare Settings. Washington, DC: Department of Health and Human Services; 2009.
2.8 How do research scientists determine efficacy for killing or deactivation of different microorganisms and viruses?
The most fundamental concept in photobiology is the action spectrum (or relative response) for a given effect. Although there is a standardized germicidal action spectrum in the IES Handbook,[12] it was based on inactivation of E. coli bacteria, and action spectra for spores, other bacteria, and different viruses can vary. This standardized action spectrum extends from 235 nm to 313 nm and peaks at approximately 265 nm. A wavelength of 254 nm has a relative efficacy of 0.85; by contrast, 313 nm in the UV-B has a relative efficacy of only 0.01.
Germicidal effectiveness is proportional to the exposure dose (radiant exposure, typically in millijoules* per square centimeter, mJ/cm2, or joules per square meter, J/m2), which is the product of the dose-rate (irradiance, typically in mW/cm2 or W/m2) and time (from 1 μs to several hours). A nonlinear relationship exists between UV exposure and germicidal efficacy. For example, if a certain UV exposure kills 90% of a bacterial population (frequently referred to as “one-log kill”), doubling the exposure time or intensity can kill only 90% of the residual 10%, for an overall germicidal efficacy of 99% (“two-log kill”). Likewise, a 50% decrease in dose or exposure time decreases germicidal efficacy only from 99% to 90%.
Humidity can reduce the effectiveness of germicidal UV radiation. There is a reference dose to attain a survival of 37%; however, in practice a GUV dose of interest is 3 or 4 log-kills, corresponding to 99.9% or 99.99% inactivation, respectively. To be effective in practice, achieving two log-kills (99% inactivation) is frequently accepted.
[12] DiLaura D, Houser K, Mistrick R, Steffy S (editors). The Lighting Handbook, 10th ed. New York: Illuminating Engineering Society; 2011.
* One joule is equal to one watt times one second. (Or, 1 W = 1 J/s) A millijoule is one-thousandth of a joule.
3.0 Disinfecting Room Air with GUV
3.1 What is upper-room GUV?
Upper-room GUV is a safe means of air disinfection that is possible in rooms with high ceilings. In this method, specially designed and installed UV-C fixtures that irradiate only the air above 2.1 meters (7 feet) constantly disinfect the upper air volume. This is most effective when there is constantly mixed air by fans and HVAC ventilation, but even without strong ventilation or fans, air constantly mixes by movements and normal convective currents.
3.2 Why is upper-room GUV more effective than UV in ventilation ducts or in room air cleaners?
Upper-room GUV (see Figure 3-1) disinfects large volumes of room air (above occupants’ heads) at once, resulting in high “equivalent” air changes per hour (ACH) in terms of air disinfection only—GUV does not dilute odors or CO2, the main functions of building ventilation. Odor control and CO2 removal are accomplished by relatively low levels of ventilation (1 to 2 ACH), but air disinfection requires much higher rates of ventilation (6 to 12 ACH), or the equivalent produced by upper-room GUV. Two hospital controlled studies [13, 14] have shown upper-room GUV to be about 80% effective against tuberculosis (TB) spread. Even when GUV is confined to the upper room, good air mixing (ideally with low-velocity ceiling fans but easily accomplished by other types of forced-air ventilation) results in very high equivalent ACH in the lower, occupied space—estimated to be an additional 24 ACH in a South African study.[13]
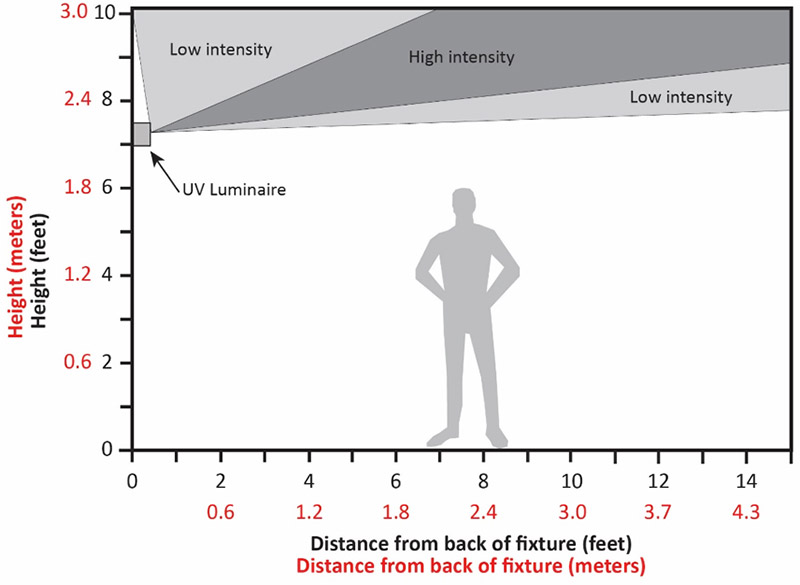
Figure 2-1. Upper-air GUV installation. [13] Mphaphlele M, Dharmadhikari AS, Jensen PA, Rudnick SN, van Reenen TH, Pagano MA, Leuschner W, Sears TA, Milonova SP, van der Walt M, et al. Institutional tuberculosis transmission. Controlled trial of upper room ultraviolet air disinfection: A basis for new dosing guidelines. Amer J Respir Crit Care Med. 2015;192(4):477-84.
[14] Miller SL. Upper room germicidal ultraviolet systems for air disinfection are ready for wide implementation (editorial). Am J Respir Crit Care Med. 2015;192(4):407-9.
3.3 Is GUV inside air ducts sufficient for room-air disinfection?
When UV is used in ducts, although it ensures that recirculated air does not have viable pathogens, it unfortunately does relatively little to prevent person-to-person transmission in a room where both an infectious source and other susceptible persons share the same air. For effective interruption of transmission, air disinfection has to occur in the same room where transmission is occurring. Portable air cleaners can be placed in rooms where there is a risk of transmission, but moving large volumes of air through any device is difficult, limited by the clean-air delivery rate of the portable air cleaner. Often when the clean air delivery rate is converted to equivalent ACH, the result is a disappointing 1 to 2 ACH, far too little to effectively prevent transmission. A large air cleaner in a small room may be effective, but for larger rooms, air cleaners are simply an impractical approach to high levels of air disinfection, compared to upper-room GUV. Air cleaners may have value in a confined space where GUV is desired.
3.4 If the room has glass that permits vision into the room and a view of the UV fixtures, does that glass need to be shuttered or covered?
No, not for safety if they are normal 254-nm UV-C lamps. Glass windows block potentially hazardous UV-B and UV-C transmission. Glass windows should be covered if pulsed xenon lamps are in use. Note: There is certainly no reason for concern with upper-air installations, since potentially hazardous UV-C does not reach the lower room.
4.0 Disinfecting Surfaces, Masks, and Instruments with GUV
4.1 How useful are UV-C rays in disinfecting surfaces?
While UVGI (UV-C in the appropriate range; see Section 1) is an excellent surface disinfectant, it does not penetrate surfaces and cannot disinfect soiled surfaces. The inability of the UV radiant energy to reach shadowed recesses of surfaces or to penetrate coverings like dust and other matter may negatively affect disinfection. For these reasons, UVGI is typically used as a supplemental control measure for disinfection. A 2005 published study concluded that UVGI lamps could have some effect on the spread of infectious respiratory diseases, but there was inadequate evidence to support recommending its wide use.[8] The CDC recognizes that UVGI has several potential applications but also has limitations and possible safety issues.[9,10,11]
[8] Lee T, Jordan NN, Sanchez JL, Gaydos JC. Selected nonvaccine interventions to prevent infectious acute respiratory disease. Am J Prev Med. 2005;28(3):305-16.
[9] Sehulster L, Chinn RYW. Guidelines for environmental infection control in healthcare facilities – Recommendations of the Centers for Disease Control and the Healthcare Infection Control Practices Advisory Committee (HICPAC). 2003;52(RR10):1-42.
[10] Jensen PA, Lambert LA, Lademarco MF, Ridzon R. 2005. Guidelines for preventing the transmission of Mycobacterium tuberculosis in health-care settings, 2005. Morbid Mortal Weekly Rep. 2005;54(RR17):1-141.
[11] Centers for Disease Control and Prevention; and National Institute for Occupational Safety and Health. Environmental Control for Tuberculosis: Basic Upper-Room Ultraviolet Germicidal Irradiation Guidelines for Healthcare Settings. Washington, DC: Department of Health and Human Services; 2009.
4.2 Can GUV be used to disinfect surgical masks and the N95 respirator mask?
Hydrogen peroxide (H202)-vapor disinfection has been the most recommended method now in use. However, if this is not available, studies by several laboratories have shown surprisingly effective UV disinfection despite the fact that UV photons will not have a straight-line pass through all the porous filter structure. Therefore, forward-scattered photons have to penetrate the mask, and substantial doses are required.[15] This should only be attempted within a light-tight enclosure. In the U.S., NIOSH and the FDA have issued temporary guidance on this important subject.[11, 16]
[11] Lindsley WG, Martin SB, Thewlis RE, Sarkisian K, Nwoko JO, Mead KR, Noti JD. Effects of ultraviolet germicidal irradiation (UVGI) on N95 respirator filtration performance and structural integrity. J Occup Environ Hygiene. 2015;12(8):509-17.
[15] Lindsley WG, Martin SB, Thewlis RE, Sarkisian K, Nwoko JO, Mead KR, Noti JD. Effects of ultraviolet germicidal irradiation (UVGI) on N95 respirator filtration performance and structural integrity. J Occup Environ Hygiene. 2015;12(8):509-17.
[16] U.S. Food and Drug Administration. Enforcement Policy for Sterilizers, Disinfectant Devices, and Air Purifiers during the Coronavirus Disease 2019 (COVID-19) Public Health Emergency – Guidance for industry and Food and Drug Administration staff. Washington, DC: FDA; 2020 Mar.
4.3 Are GUV wands effective for disinfecting surfaces?
Hand-held, compact GUV products (see Figure 4-1) have been marketed for more than a decade for disinfecting small objects such as cell phones. Most of these emit less than 2 mW·cm-2 of 254-nm UV-C at contact, meaning that the wand has to be held to the surface for several seconds for an effective multi-log unit disinfection. Waving it over an object such as a postcard for one second will not provide reliable disinfection. These products typically employ a safety switch that senses when the emission is not directed downward (away from the eyes) and shuts off if turned upward. Even if safely used, these might provide a false impression of effective disinfection.

Figure 4-1. Small UV-C mercury lamps and 270-nm LEDs used in hand-held wands are available on the internet (middle and bottom). Small air-space disinfectant units (top) are also sold.
(Image courtesy of David Sliney)
5.0 GUV Safety
5.1 Are GUV lamps safe?
UVGI lamp emissions can pose a workplace safety and health hazard to the eyes and skin if the lamps are improperly used or installed. However, these lamps can be used safely if workers are informed regarding the hazards and follow appropriate precautions. Upper-room GUV has been safely used for preventing airborne transmission for at least 70 years. A great deal is known about the human exposure limits of 254-nm UV (UV-C) irradiation. Compared to the UV-A and UV-B in sunlight, UV-C is almost entirely absorbed by the outer dead layer (stratum corneum) and outer skin (outer epidermis), with very limited penetration to the deeper cellular layers of skin where new cells are constantly created. For comparison, the current daily safety limit of 254-nm UV-C for 8 hours is 6.0 mJ/cm2, whereas less than ten minutes of summer sun exposure at a UV Index of 10 can deliver the equivalent limiting daily safety dose[17] because of its much more-penetrating UV-A and UV-B. A study of continuous monitoring of healthcare workers and patients in an upper-air GUV installation recorded no more than 1/3 of the 8-hour dose. Because it has no outer dead protective layer, the human eye is the organ most susceptible to sunlight and upper-room GUV. Exceeding the threshold level value (TLV) in the lower room will result in painful irritation of the cornea similar to overexposure on a sunny day, especially from sun reflected from water or snow. The damage is painful but transitory, with corneal shedding and replacement in a day or two. When the UV-C source is overhead, the eyes receive very little exposure during normal activities; this is demonstrated in sunlight when the sun is overhead—there is hazardous exposure of the skin but not the eyes. There are no known long-term consequences from an accidental UV-C overexposure.[18] Most eye injuries result from workers on ladders cleaning fixtures or working in the upper room without first turning off the fixtures.[19] For this reason, only trained maintenance workers should be working in the upper room or replacing in-duct lamps. Eye injuries have resulted from insufficient training or improper installation—e.g., workers mistakenly installing an upper-room UVGI fixture upside-down after bulb replacement.[20]
[17] American Conference of Governmental Industrial Hygienists. 2020 Threshold Limit Values and Biological Exposure Indices. Cincinnati: ACGIH; 2020.
[18] International Commission on Illumination (CIE). CIE 187:2010, UV-C Photocarcinogenesis Risks from Germicidal Lamps. Vienna: CIE; 2010.
[19] Sliney D. Balancing the risk of eye irritation from UV-C with infection from bioaerosols. Photochem Photobiol. 2013;89(4):770-6. [Erratum in: Photochem Photobiol. 2013 Jul-Aug; 89(4):770].
[20] Sensakovic JW, Smith LG. Nosocomial ultraviolet keratoconjunctivitis. Infect Control. 1982;3:475-6.
5.2 Are there safety rules for GUV surface-disinfection lamps?
To ensure the safe use of UVGI lamps for surface disinfection, follow these guidelines:
- All lamps. Workers should place temporary warning signs at access points to the area being disinfected. They should either vacate the area during disinfection or place opaque barriers between the UVGI lamp and room occupants. If these areas are required to be occupied during disinfection and exposures cannot be avoided (e.g., if using a handheld disinfecting UVGI “wand”), then personal protective equipment (PPE) should be used.
- Low- and medium-pressure mercury lamps, UVGI LEDs, and far UV-C lamps. Workers should wear plastic or glass face shields to protect the eyes and face, nitrile gloves or work gloves to protect the hands, and full-coverage clothing with tightly woven fabrics to protect all other exposed skin.
- Pulsed xenon arc lamps. Workers should wear welding or cutting goggles to protect the eyes, nitrile gloves or work gloves to protect the hands, and full-coverage clothing with tightly woven fabrics to protect all other exposed skin.
5.3 Do eye or skin hazards differ depending upon the lamp type used?
Low-and medium-pressure mercury UVGI lamps emit UV energy that poses a hazard to the cornea and skin. Some UVGI LED devices emit near 270 nm, which poses a hazard to the cornea and skin. “Far UV-C” lamps that emit around 222 nm can pose a hazard to the cornea, and recent studies have been inconsistent regarding whether far UV-C lamps pose a significant skin hazard.[22, 23] Differences may be the result of different glass envelopes allowing some longer-wavelength radiant-energy transmission.
Pulsed xenon arc UVGI lamps emit UV and visible radiant energy that poses a hazard to the retina, cornea, and skin. Some pulsed xenon arc lamps are filtered so that only the UV energy for disinfection is emitted. Xenon arc lamps can also pose additional safety hazards if they are not maintained properly. These GUV lamps are generally used only in industry, to sterilize food and pharmaceutical containers, for example, but also have been used in GUV robots for hospital room disinfection. Maintenance and service should only be performed by authorized persons.
[22] Buonanno M, Ponnaiya B, Welch D, Stanislauskas M, Randers-Pehrson G, Smilenov L, Lowy FD, Owens DM, Brenner DJ. Radiation Res. Germicidal efficacy and mammalian skin safety of 222 nm light. 2017;187:493-501.
[23] Woods JA, Evans A, Forbes PD, Coates PJ, Gardner J, Valentine RM, Ibbotson SH, Ferguson J, Fricker C, Moseley H. The effect of 222-nm phototesting on healthy volunteer skin: A pilot study. Photodermatol Photoimmunol Photomed. 2015;31:159-66.
5.4 Are there safety rules for GUV air-disinfection lamps?
To ensure the safe use of UVGI lamps for air disinfection, follow these guidelines:
- All lamps. Workers should place warning signs near upper-room UVGI lamps and on AHU access panels where internal UVGI lamps are installed. Activation switches should be clearly labeled and protected with switch guards to prevent accidental activation by unauthorized personnel. If exposures cannot be avoided, workers should wear plastic or glass face shields to protect the eyes and face, nitrile gloves or work gloves to protect the hands, and full-coverage clothing with tightly woven fabrics to protect all other exposed skin.
- Upper-room UVGI lamps. Proper installation is critical to ensure the safe use of these lamps. It is important that ceiling reflectance at the UV-C wavelength be studied before installing in a new location, since down-welling UV-C could be increased. Regular work activity should not resume in rooms with upper-room UVGI lamps unless qualified measurements have confirmed that the potential radiant exposures in the lower room are within the 8-hour exposure limits specified by the ACGIH.[17] Except in very large rooms, the emitting lamps should not be visible to occupants in the lower room.
- AHUs with internal UVGI lamps. Access panels for AHUs with internal UVGI lamps should be interlocked with automatic shutoff switches to prevent accidental exposure to UV radiant energy. An inspection window that blocks germicidal UV energy (e.g., plastic or glass) should be installed to allow workers to see whether the UVGI lamp inside the AHU is operating.
[17] American Conference of Governmental Industrial Hygienists. 2020 Threshold Limit Values and Biological Exposure Indices. Cincinnati: ACGIH; 2020.
5.5 Will GUV increase my lifetime risk for skin cancer?
UV-C penetrates only the superficial layers of the skin and eye, with the shortest wavelengths hardly penetrating at all to living cells (epidermis), so only a very mild, transitory “sunburn” (erythema) occurs from accidental over-exposure of skin areas. Even though GUV lamps can pose a theoretical delayed hazard, incidental UV exposures in the workplace would not significantly increase one’s lifetime risk for cataract or skin cancer when compared to daily exposure to the UV radiant energy in sunlight. Solar UV is much more penetrating and reaches the germinative (new-cell producing) layers in the skin, with the result that skin cancer risk is significant, and sunburns can be severe. There is a small amount of UV-B (297, 303, 313 nm) from a low-pressure mercury lamp, but this is insignificant unless exposures are experienced at least an order of magnitude or more above the safety limits for 254 nm.[18]
[18] International Commission on Illumination (CIE). CIE 187:2010, UV-C Photocarcinogenesis Risks from Germicidal Lamps. Vienna: CIE; 2010.
6.0 Lamp Technologies
6.1 What types of lamp sources are used for GUV?
Lamp technologies include continuously emitting low- and medium-pressure mercury lamps, as well as pulsed xenon arc lamps. Studies have shown that these technologies—continuously emitting or pulsed—are comparably effective for disinfection. Pulsed sources may be more practical if rapid disinfection is required.[21] Light emitting diodes (LEDs) and krypton-chlorine excimer lamps, which emit in narrow bands in the germicidal range (UV-C), are emerging technologies.
[21] Wang T, MacGregor SJ, Anderson JG, Woolsey GA. Pulsed ultra-violet inactivation spectrum of Escherichia coli. Water Res. 2005;39(13):2921-5.
6.2 What is currently the most widely used lamp source of UV-C for GUV?
The most practical method of generating germicidal radiant energy is by passage of an electric discharge through a rare gas (usually argon) at low pressures (on the order of 130 to 400 pascals, or 1 to 3 torr) containing mercury vapor enclosed in a special glass tube with no fluorescent coating that transmits short-wavelength UV. Hot-cathode germicidal lamps are identical in shape, electrical connection, operating power, and life to standard fluorescent lamps, both linear and compact types. Maintaining the transmission of the lamp over life is more difficult than for standard fluorescent lamps.
Cold-cathode germicidal lamps are also available in various sizes, usually for shorter, smaller diameter lamps. Their operating characteristics are similar to those of hot-cathode lamps, but their starting mechanisms are different
Approximately 45% of the input power from such a device is emitted at a mercury-discharge wavelength of 253.7 nm, in the middle of the UV-C band. The second major emission line is at 184.9 nm, but this emission is normally absorbed by the glass, since—if emitted through the glass, as it is with pure quartz—it would create ozone at levels far above the safety limit. Other mercury lines in the UV-B and UV-A regions are present at much lower emitted-power levels and not considered important in germicidal action; unfortunately, they can add to the safety concern.
6.3 Are there higher-output UV-C lamps?
Medium pressure mercury (Hg) lamps are also used, particularly in water purification. Such lamps resemble high pressure mercury lamps—i.e., are much more compact—and use a clear or doped quartz envelope, depending on application. While the efficiency of the 253.7-nm emission is significantly reduced and broadened due to reabsorption of the radiant energy, it is nevertheless an important source, as it can be operated at much higher power per unit length than low pressure mercury lamps.
Other sources, such as rare gas-halogen (e.g., krypton-chlorine, Kr-Cl) discharge, have been shown to produce significant emission in the far UV-C region (205 to 230 nm). The advantage of sources such as those emitting 207 nm or 222 nm, is that the deactivation rate of some bacteria and viruses appears to be relatively high, and the effect of the emission on human skin and eyes is much reduced compared to the 253.7-nm mercury emission.[22] However, depending on the glass envelope, small but significant levels of longer wavelengths may be of concern.[23] At this time, such sources have been developed in the research laboratory, but their presence in the marketplace is still very limited in comparison to that of mercury lamps, and there is little experience yet with any widespread use.
[22] Buonanno M, Ponnaiya B, Welch D, Stanislauskas M, Randers-Pehrson G, Smilenov L, Lowy FD, Owens DM, Brenner DJ. Radiation Res. Germicidal efficacy and mammalian skin safety of 222 nm light. 2017;187:493-501.
[23] Woods JA, Evans A, Forbes PD, Coates PJ, Gardner J, Valentine RM, Ibbotson SH, Ferguson J, Fricker C, Moseley H. The effect of 222-nm phototesting on healthy volunteer skin: A pilot study. Photodermatol Photoimmunol Photomed. 2015;31:159-66.
6.4 Are there UV-C emitting LEDs available?
There are reports of companies developing LEDs that emit in the longer-wavelength UV-C region, generally at 265 to 270 nm. As yet, complete upper-air systems are not on the market, but with the focus of the SARS-CoV-2 novel coronavirus pandemic upon us, these may become a reality in the future.
7.0 GUV Applications
7.1 How much UV “light” is required, and how long does the process take, to disinfect a volume of air or a surface?
There are very sophisticated programs to calculate the lamp sizes and in-air dose requirements in terms of energy required for space and radiant fluence (joules per square meter, J/m2) across a cross-section of a UV-C beam, but there is a much simpler evidence-based dose that has been developed over many years for TB control, typically specified as about 17 mW of 254-nm lamp-emission radiant power per cubic meter (m3) of space to disinfect air.[13] Although this sounds too simplistic to be true, since air in any room is always moving and mixing, one can correctly assume that all air will be treated—the better the air mixing, the sooner this will happen. Studies at the Harvard School of Public Health[13, 14] and elsewhere show log units of reduction equivalent to 24 ACH to achieve 80% reduction of transmission. Of course, 100% reduction is not possible, because of the multiple modes of transmission. To disinfect surfaces, this depends on the type of surface and its cleanliness; recommended exposures vary from 200 to 1,000 J/m2 (20 to 100 mJ/cm2).[24]
[13] Mphaphlele M, Dharmadhikari AS, Jensen PA, Rudnick SN, van Reenen TH, Pagano MA, Leuschner W, Sears TA, Milonova SP, van der Walt M, et al. Institutional tuberculosis transmission. Controlled trial of upper room ultraviolet air disinfection: A basis for new dosing guidelines. Amer J Respir Crit Care Med. 2015;192(4):477-84.
[14] Miller SL. Upper room germicidal ultraviolet systems for air disinfection are ready for wide implementation (editorial). Am J Respir Crit Care Med. 2015;192(4):407-9.
[24] Jelden KC, Gibbs SG, Smith PW, Schwedhelm MM, Iwen PC, Beam EL, Hayes AK, Mar4on N, Kratochvil CJ, Boulter KC, et al. Nebraska Biocontainment Unit patient discharge and environmental decontamination after Ebola care. Amer J Infect Control. 2015;43(3):203-5.
7.2 How can I measure the light to make sure I’m getting the appropriate amount to get effective disinfection?
There are a number of dedicated meters available; however, a wide range of scale is normally required, e.g., a range from 0.1 to 100 microwatts per square centimeter (µW·cm-2).[25] Safety readings require the lower range, and efficacy requires a range up to at least 10 mW·cm-2. A common practice is to have two calibrated meters: one in reserve and for reference. The two instruments should be periodically compared. The user should retain the manufacturer’s instructions, including a description of the meter, its safe use, and maintenance and calibration of it. Some healthcare facilities contract with a full, outside maintenance contractor that uses calibrated meters and correctly and safely replaces burned-out lamps. Some users retain a simple, less precise meter for staff to use, but the installer uses a professional meter.[26]
[25] Reed NG, Wengraitis S, Sliney DH. Intercomparison of instruments used for safety and performance measurements of ultraviolet germicidal irradiation lamps. J Occup Environ Hyg. 2009;6(5):289-97.
[26] End TB Transmission Initiative. Maintenance of Upper-Room Germicidal Ultraviolet (GUV) Air Disinfection Systems for TB Emission Control. Copenhagen: United Nations Office for Project Services (UNOPS); 2020. Available online: http://www.stoptb.org/wg/ett/. (Accessed 2020 Apr 12).
7.3 Can GUV lamps be safely installed in hospital tents?
Press reports show installation of UV-C lamps in hospital tent ceilings (whole-room GUV) where all persons were fully protected by infection-control head and face coverings, gloves, and coveralls. This should have been safe if all complied with complete protective covering. Upper-air disinfection should not be ruled out if hospital tents are quite high and sufficient airspace above 2.1 m (7 ft) is available, but the special upper-air GUV fixtures would have to be very stable so as to not tip and thereby direct GUV downward into occupied spaces.
7.4 Can less-louvered fixtures be used in very high-ceiling (high-bay) areas?
Yes, with high-bay areas, high-ceiling warehouses, or high-ceiling marketplaces, a highly louvered UVGI fixture should not be required. Instead, much more efficient, properly installed open-lamp fixtures—wall mounted or suspended—are quite effective. (Note: This was common in industrial sites many decades ago.) The UV radiant energy is all directed upward, as shown in Figure 7-1. Low-velocity ceiling fans (not shown) ensure good vertical air movement.
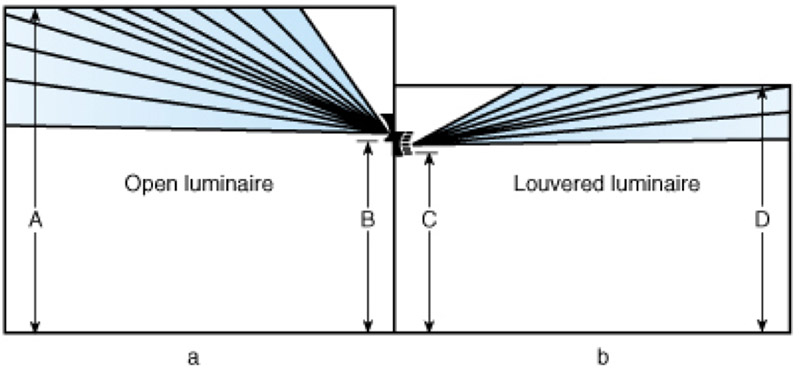
Figure 7-1. Germicidal lamps for air disinfection in occupied rooms: (a) open unit used in rooms over 3 m (10 ft) in height; (b) louvered unit used where ceilings are lower than 3 m (10 ft). Dimensions: A, 6 m (20 ft); B, 3 m (10 ft); C, 2.1 m (7 ft); D, 3 m (10 ft). (Source: The Lighting Handbook12 [12] DiLaura D, Houser K, Mistrick R, Steffy S (editors). The Lighting Handbook, 10th ed. New York: Illuminating Engineering Society; 2011.
7.5 Are there standards that address testing of GUV lamps in air ducts?
ASHRAE publishes two method of test standards to evaluate UV equipment:
- ASHRAE Standard 185.2-2014, Method of Testing Ultraviolet Lamps for Use in HVAC&R Units or Air Ducts to Inactivate Microorganisms on Irradiated Surfaces[27]
- ASHRAE Standard 185.1-2015, Method of Testing UV-C Lights for Use in Air-Handling Units or Air Ducts to Inactivate Airborne Microorganisms[28]
[27] ASHRAE. Standard 185.2-2014, Method of Testing Ultraviolet Lamps for Use in HVAC&R Units or Air Ducts to Inactivate Microorganisms on Irradiated Surfaces. Atlanta: ASHRAE; 2014.
[28] ASHRAE. Standard 185.1-2015, Method of Testing UV-C Lights for Use in Air-Handling Units or Air Ducts to Inactivate Airborne Microorganisms. Atlanta: ASHRAE; 2015.
7.6 Can GUV be used in the home?
As described in Section 4.3, handheld, compact GUV products (see Figure 4-1) are sold but are considered a serious safety concern in a general household environment, where children, pets, or careless adults can easily be overexposed. These products are typically less than watts, with open and exposed mercury lamps. They may come with a safety timer; a person places the open lamp on a table or in a convenient location, sets the timer for several minutes to an hour, and is given a 10-second delay to quickly exit the room and close the door.
7.7 Does UV degrade paints and other wall materials, or hurt plants?
UV rays in general will degrade paint, yellow plastics, and destroy air filters based on their composition (thus, UV-C irradiation of respirators for reuse should be only be a last resort in a pandemic). Furthermore, shorter-wavelength UV photons have higher energy potential than longer-wavelength UV photons, and may have an accelerated aging effect on materials and paints. UV-C may damage plants; therefore, hanging plants should not be placed in the disinfection zone in upper-room applications or in whole-room UV-C applications.
7.8 How effective are UV robots for surface disinfection?
Hospitals and healthcare facilities have rooms that can be closed off to individuals for a length of time. So-called “UV-C robots” have been used to move around a room to disinfect surfaces with UV-C in all directions. The UV-C radiant energy is normally emitted by long, vertical mercury lamps or pulsed xenon lamps. It is a challenge to estimate dose, but very intense emission can cover much of the room in a relatively short time. Further, by moving autonomously around the unoccupied work space it can expose surfaces that would not be easily reached by fixed GUV lamp installations. If good air movement is present, most air will be disinfected as well, and the dose requirements noted in the answer to the previous question could be applied. Surfaces with thick buildup of residues may pre-absorb the UV-C photons before they reach the active virus or bacterium. As with all GUV systems, they should be considered as an effective adjunct to standard infection control cleaning guidance. These mobile units should be used after terminal cleaning of patient rooms and bathrooms.[25, 29]
[25] Reed NG, Wengraitis S, Sliney DH. Intercomparison of instruments used for safety and performance measurements of ultraviolet germicidal irradiation lamps. J Occup Environ Hyg. 2009;6(5):289-97.
[29] Anderson DJ, Chen LF, Weber DJ, Moehring RW, Lewis SS, Triplett PF, Blocker M, Bechererm P, Schwab JC, Knelson LP, et al. Enhanced terminal room disinfection and acquisition and infection caused by multidrug-resistant organisms and Clostridium difficile (the Benefits of Enhanced Terminal Room Disinfection study): A cluster-randomised, multicentre, crossover study. Lancet. 2017;389(10071):805-14.
7.9 What do upper-room GUV systems cost?
A summary of cost considerations is available from the End TB Transmission Initiative.27
[27] ASHRAE. Standard 185.2-2014, Method of Testing Ultraviolet Lamps for Use in HVAC&R Units or Air Ducts to Inactivate Microorganisms on Irradiated Surfaces. Atlanta: ASHRAE; 2014.
